Quick Read:
- Fasting is not a blanket solution for all women, especially during breast cancer healing. Always TEST so you know exactly what your body needs.
- Testing transforms fasting (and all healing therapies) from a trend into a targeted strategy—or gives you data-backed permission to let it go if it’s not a good fit.
- For some women, during certain times of their lives, fasting may: increase thyroid issues, throw off hormone balance, spike cortisol levels, prevent quality sleep, decrease cognitive functionality, and provide many other damaging effects.
For about a decade now, Intermittent fasting (IF) has been a highly praised trend that has been claimed to improve metabolic health, help maintain weight loss, increase longevity, and even prevent cancer.
But is it just hype? Should everyone do it? Is it something that Wellness Warriors should be doing? Is it safe for breast cancer healing? Will it impact my hormones?
Those questions and more are all ones you should be asking, and so are we.
While there is promising research supporting the idea that time-restricted eating can help regulate blood sugar, support autophagy (your body’s natural cellular cleanup process), and reduce inflammation, there’s an important caveat many overlook:
Fasting isn’t a one-size-fits-all solution, especially for women navigating breast cancer.
Therefore, always do what is best for YOUR body, according to testing and strategizing with your medical team.
But before we unpack why fasting may or may not be your healing hero, here’s a quick recap of a few common types of fasting
- Intermittent Fasting (IF): Various eating schedules ranging from eating every other day to only eating for 6 hours out of the day.
- Time-Restricted Eating (TRE): A flexible method that focuses on the timing of eating rather than the caloric intake. This is a form of IF.
- Complete Fast: Only drinking water for 3 days straight.
- Fasting Mimicking Diet (FMD): A patented program distributed by Dr. Longo’s company, ProLon™. [1] It is designed to provide a 5-day supply of meals once a month so that a person can achieve the autophagy and other benefits that fasting can provide while still eating a bit.
A fast history of health studies.
We are all about tuning into your body’s unique needs and genetics. That means every strategy, supplement, and therapy should align with your current situation, as determined by personalized tests. Not where a study says you “should” be. Especially studies that are only done on male bodies. That’s right. It wasn’t until 1996 [2] that it was mandatory for health and medical studies to include women.
However, the first large-scale study (encompassing 140,000 women) on intermittent fasting in women was not published until February 2023. That’s just TWO years ago, even though intermittent fasting has been all the rage since the early 2010s. This study, known as The Big IF Study [3], was funded by Zoe, a personalized nutrition program. The women also had a 10-hour eating window, and most intermittent fasters follow a 6 or 8-hour eating window.
Your Body, Your Blueprint.
Fasting might be the right fit for some, but for others, it can be counterproductive and even harmful. This is especially true if you’re already dealing with hormonal imbalances, blood sugar fluctuations, or stress from cancer treatment.
Let’s unpack why fasting is a complex decision to make—and how to personalize your approach.
Fasting and Female Hormones: A Delicate Dance
Here’s where it gets tricky. The female body is exquisitely tuned to detect energy availability, especially regarding reproduction, stress, hormonal balance, and menstrual cycles (if you still have one)
Some studies have shown that caloric restriction from fasting can have the following harmful impacts on some women’s bodies:
- Disrupt menstrual cycles
- Lower estrogen levels [4]
- Trigger ovulation problems
- Lead to fertility issues
- Cause fatigue, irritability, and blood sugar crashes [5]
- Increase stress and cortisol in the body, damaging your immune, nerve, and adrenal systems [6]
- It restricts the fuel needed for optimal cognitive function
- Increase thyroid issues [7]
Women in peri-menopause or menopause are especially vulnerable because they’re already navigating declining estrogen and progesterone. Adding fasting into the mix without proper support may further disrupt this balance.
As discussed in this insightful video from Dr. Beth Westie [8], fasting may lead to more harm than good for some women. It causes even more stress on the body during a time when your body is already facing immense stress due to treatment, medications, therapies, and managing everything else in your life.
The Case for Personalized Testing
Testing is your superpower.
Fasting might benefit someone who is insulin-resistant, has elevated fasting glucose, or struggles with obesity. But for someone who is already lean, active, and not metabolically inflexible, fasting could inc [5]rease cortisol, slow thyroid function, and disrupt estrogen balance. All of which prevent breast cancer healing. Hence, the importance of testing and not guessing when it comes to your health.
[5]rease cortisol, slow thyroid function, and disrupt estrogen balance. All of which prevent breast cancer healing. Hence, the importance of testing and not guessing when it comes to your health.
Here are a few key markers that can help determine if fasting is beneficial for you:
- Fasting glucose and insulin levels. Click here [5] to learn how to test your insulin levels and blood sugar, and then read this blog [9] to uncover the breast cancer and blood sugar connection.
- Hemoglobin A1c. You can easily order this test from YourLabWork’s Metabolism Test. [10]
- Cortisol levels via saliva, blood, or urine. The Comprehensive Plus Hormone Profile [11] is a great option.
- Thyroid function (TSH, free T3, free T4). Click here [7] to learn about Dr. V’s thyroid and breast cancer connection. We suggest ordering Dr. V’s full Thyroid Panel [10].
- Hormone panel (estrogen, progesterone, DHEA). You can also order these from YourLabWork [10] or your doctor.
Knowing your numbers can help eliminate the guesswork from your healing process. That’s why we always say: TEST. Don’t Guess and Stress. Testing transforms fasting (and all healing therapies) from a trend into a targeted strategy—or gives you data-backed permission to let it go if it’s not a good fit.
Alternative Strategies To Fasting
If you’re curious about fasting but cautious, here are a few more balanced options to explore:
1. Try a 12-Hour Overnight Fast
Stop eating after dinner (say, 7pm) and eat breakfast around 7am. This is often enough to support healthy digestion and repair without stressing the body.
2. Eat Before Workouts
Especially for women, exercising in a fasted state can spike cortisol, causing damage to DNA, the immune system, and the adrenal glands, and prevent the body from recovering. If you’re active, aim for a light meal that includes protein and quality carbohydrates before your morning workout.
3. Listen to Your Cycle (If You Still Have One)
Women are more sensitive to caloric restriction during the luteal phase (after ovulation). Consider easing up on fasting during this time and supporting your body with more nourishing, grounding foods.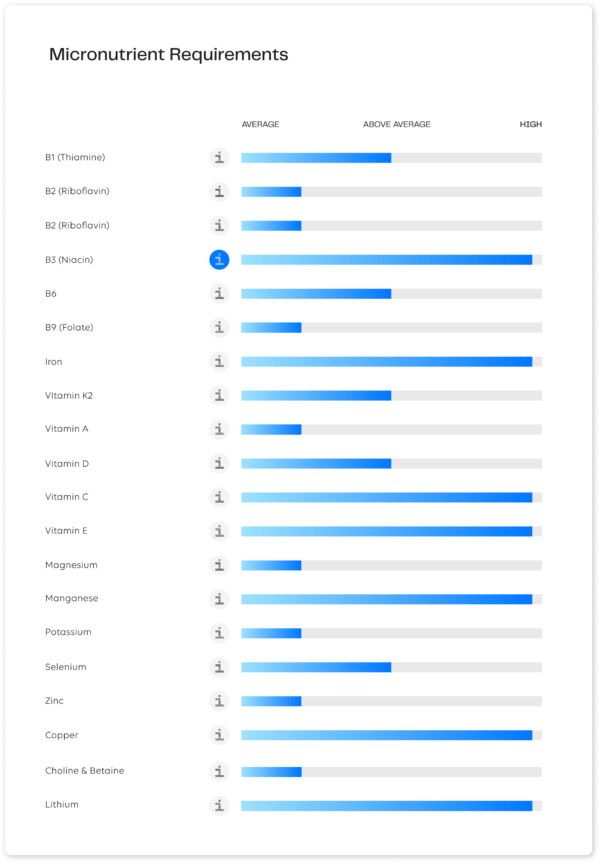 [12]
[12]
4. Focus on Nutrient Timing
Even if you’re not fasting, you can support healing with what you eat and when. Prioritize eating that best aligns with your circadian rhythms, cycles, and genetic makeup. You can find out exactly what you need through the Nutrition Genome test. (See sample results graphic on the right for an example of the personalized data the test offers.)
In summary: Fasting is not “bad,” but it’s not a blanket solution for all women, especially during breast cancer healing.
Fasting may have a place for some, but it may not be helpful for your unique journey. Support your body in a way that feels balanced, sustainable, and grounded in your unique needs.
Listen to your body; it will always tell the truth.
Your Next Read: Are There Protein Deficiencies In Plant-Based Diets? [13]