As you know, I am all about VERY EARLY DETECTION (Essential #7 [1])! The earlier you can detect, the sooner you can change your lifestyle and closely monitor changes. Thus, beginning the healing process and your new life of vibrant health! A key to early detection is knowledge about different types of testing and what could be found in the test results. Breast calcifications are common findings in mammograms, and inflammation from breast calcifications can be detected in thermography.
My soap box moment: While mammograms have their place and can be helpful, they are NOT the only test available! In fact, the radiation from the test can cause DNA damage which could increase your risk of breast cancer. The poking, prodding, and squishing that is involved in a mammography exam may rupture small tumors if they exist—causing cancer cells to spread throughout the body. Additionally, by the time a mammogram can detect cancer, a patient may have had tumor growth for up to 8 years!
However, fear not—there are safe, painless, noninvasive, and incredibly effective tests that you can use. Please check out: thermography [2], Galleri Test, RGCC Test [3], Prenuvo Test, and SonoCine Test [4]. For further reading, please check out how DCIS Stage 0 treatments [5] can actually lead to developing breast cancer!
And now, back to our breast calcifications class!
What Are Breast Calcifications?
Breast calcifications are calcium deposits [6] that often develop in your breast tissue. It can happen when abnormal cells grow unchecked inside the duct. The cells may get so crowded that some of them die, and your body can’t clear them away. This leads to those cells hardening (petrifying), and tiny areas of calcium forming in your breast tissue. Almost all of the time, breast calcifications are painless and too small to feel with your fingers.
Breast calcifications are so common that half of all women over age 50 will have some type of calcification show up on their mammogram. They are not anything to fear at all because the vast majority will be non-cancerous. The other small percentage may turn into DCIS Stage 0 [5] at some point. For all types of breast calcification, you can just let them be and observe. You typically do not need to do any sort of treatment, but discuss this with your doctor.
Calcium & Confusion
Don’t also get hung up on the name and worrying about your calcium intake causing calcifications. You can’t get breast calcifications by having too much calcium in your diet or taking too many calcium supplements.
Calcium can be a confusing topic as well. Have you ever had these questions?
- Is there a difference between bone density and bone strength?
- Should I drink milk “for strong bones,” as countless commercials have told me?
- Do conventional calcium supplements help or hurt my breast cancer?
You aren’t alone. All of the above and more are excellent and common questions. Please check out this blog [7] post to learn my fact-based answers that are specific to breast cancer conquerors!
Skin Calcifications
No further testing is required if calcifications are clearly located in the skin rather than in the breast tissue. This could result from a powder or deodorant residue on the skin that showed up as calcifications.
The Two Types of Breast Calcifications
Macrocalcifications
Macro = large. Bigger is better in this case! Macrocalcifications are larger bits of calcium deposits that may be due to natural changes in a woman’s breast, like the hardening of her breast arteries. Macrocalcifications may also represent areas of inflammation from an old injury or breast trauma. This type is prevalent in women 50+ and benign/unrelated to breast cancer. You do not need to treat these or have them removed.
Generally, these calcifications are:
- Larger than 0.5 millimeters (mm)
- Have well-defined edges and fairly standard shapes
- Are not clustered in one area of the breast
- Some of the ways people describe them are: popcorn-like, coarse, railroad track pattern, and rim-like
Microcalcifications
Micro = small. Microcalcifications are tiny bits of calcium deposits that rarely could be an early sign of breast cancer. The most common form of cancer that could be seen from a microcalcification is ductal carcinoma in situ, which is considered Stage 0 cancer. If you have not already, please take a moment to read about how treatment for Stage 0 cancer can actually lead to developing breast cancer [5].
Generally, these calcifications are:
- Smaller than 0.5 mm each
- Vary in size and shape
- Are clustered in one area of the breast
- Some of the ways people describe them are: Spiky, irregular shapes, tight clusters
If your microcalcification is cancerous, it can help you determine treatment plans. For example, a new study [8] found that: breast cancers that have microcalcifications are more likely to be HER2-positive, tend to have a higher tumor grade, are more likely to have spread to lymph nodes, and have a greater risk of recurrence.
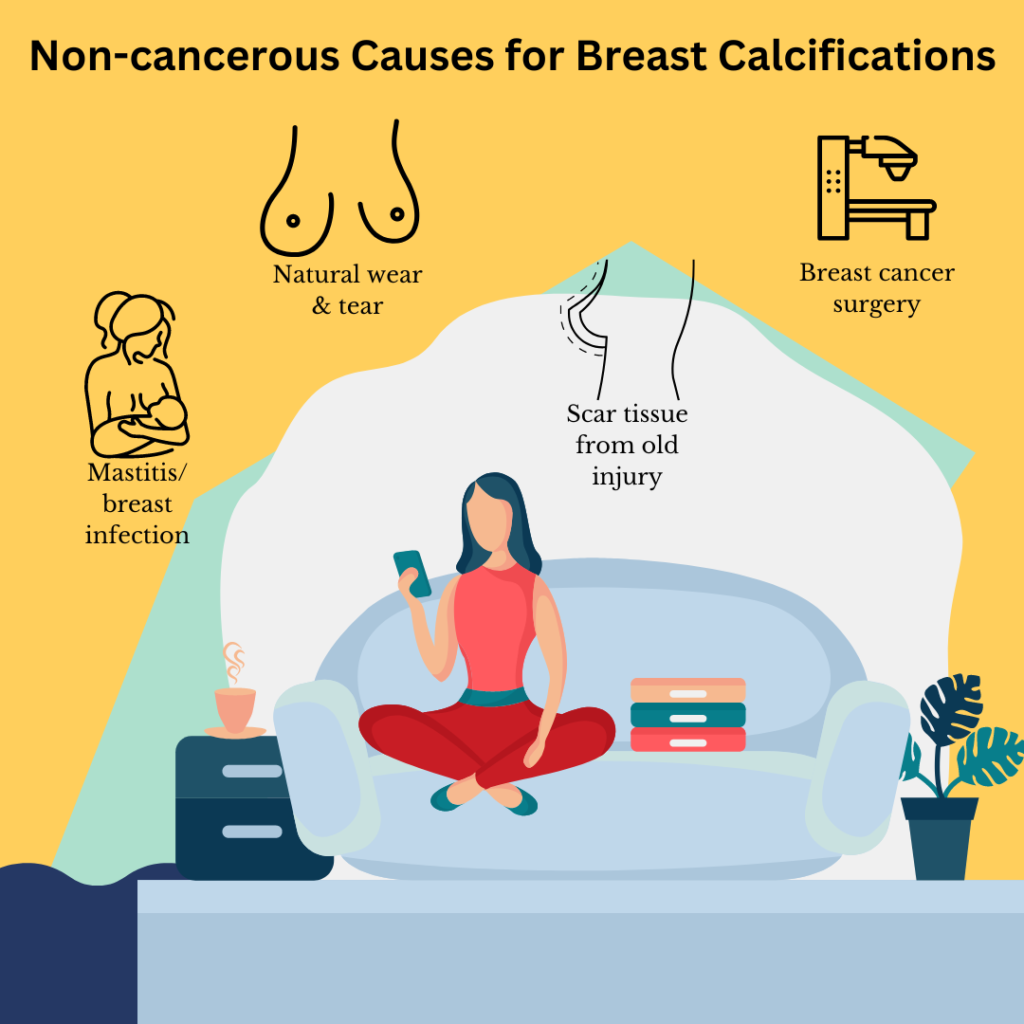
Causes of Benign Breast Calcifications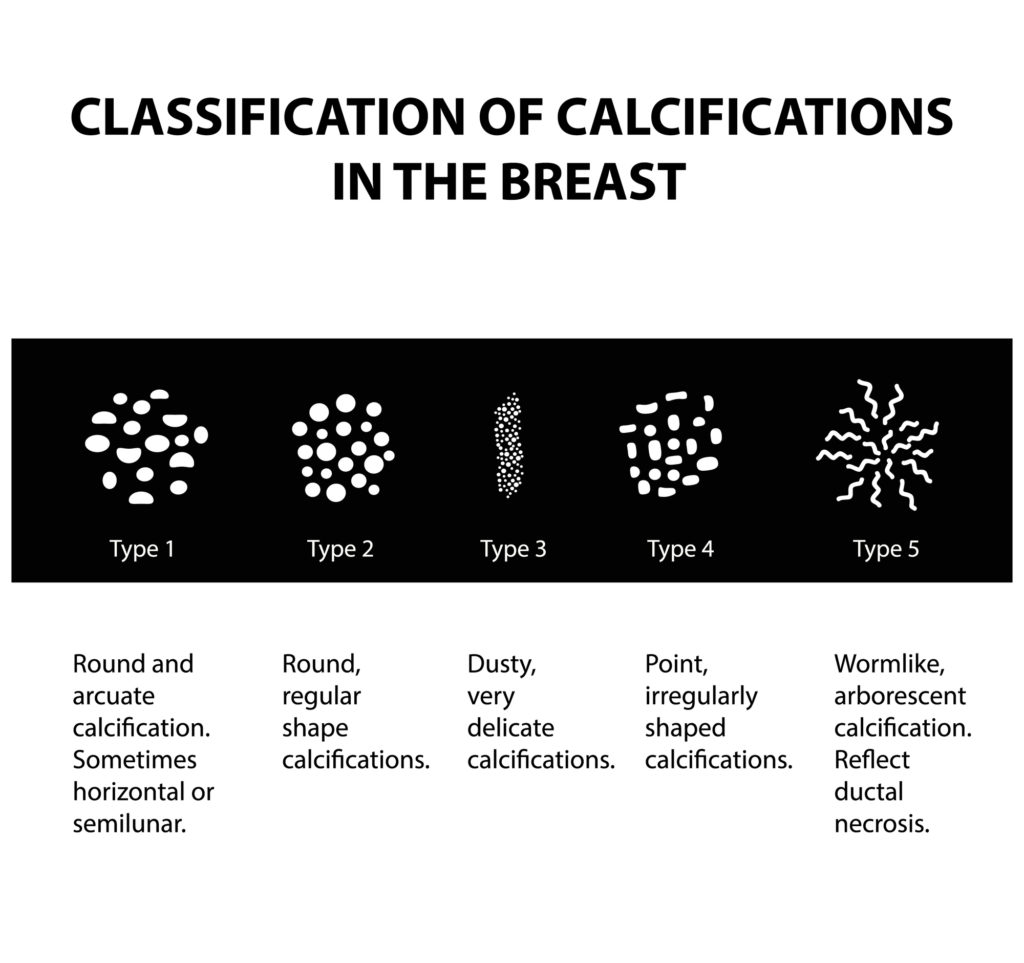 [9]
[9]
There are all sorts of reasons for these no-worries, but good-to-know-about calcification [10].
Here are a few:
- Scar tissue related to old breast injuries (dystrophic changes)
- Leftover from prior breast cancer surgery
- Natural wear and tear of the breasts
- Mastitis or inflammation caused by a breast infection
- Calcium collected inside a dilated milk duct
- Calcium mixed with fluid in a benign breast cyst
- Radiation treatment for breast cancer
- Calcifications in a fibroadenoma
Sometimes your doctor may do a biopsy to determine for sure the underlying cause of the calcium deposit. This is normal, and will just provide more info.
Arterial Calcifications and Heart Disease
Traditionally, calcifications in the arteries were thought of as incidental findings unrelated to breast cancer risk, so they were ignored. However, new research [11] is finding that presence of breast arterial calcifications IS associated with underlying coronary artery disease. This happens mainly in women over 40 who don’t have any symptoms of heart disease. The studies show an arterial calcification can be a bigger predictor of arteriosclerosis compared to standard signs such as high blood pressure or a family history of heart disease.
Oxalates in your Veggies May Cause Microcalcifications and Breast Cancer!
A study published in the BMC Cancer Journal [12] reported that “….oxalate induces proliferation of breast cells and stimulates the expression of a pro-tumorigenic gene.” They found that chronic exposure of breast epithelial cells to oxalates promoted healthy cells to turn into tumor cells! So what foods are high in oxalates? Spinach, beets, black tea, kale, chocolate, just to name a few. Does that mean that you should stop eating these healthy foods? Not necessarily. However, if you are prone to kidney stones adn have issues with breast calcifications, definitely focus on low oxalatate foods.