
Before you read this blog, please note that I am NOT suggesting that you don’t get your yearly mammograms. When I post data about mammography, I often receive angry emails and social media responses about how a mammogram saved their life by detecting breast cancer. Please note, that by the time a tumor is detected in the breast on a mammograms, it has been there for 5-8 years. And according to a 5 year Canadian study on nearly 90,000 women, mammograms were just as effective as a self-breast exam in detecting a tumor. Mammograms did NOT reduce breast cancer mortality rate at all, not even by 1%.
So now that I have laid the ground work – please read on . ![]()
In 2015, the American Cancer Society (ACS) made a surprising adjustment to their decades-old mammography recommendations. Effective in July of that year, the ACS recommended that women begin receiving annual mammography exams at age 45, not 40. The ACS also now suggests that women over 55 “cut back” on their screenings to every 2 years instead of every year.
According to the U.S. Centers for Disease Control and Prevention, approximately 67% of the U.S. female population receive a mammogram screening each year. So why did the ACS change its tune?
The 2017 Danish Study: False Positive Rates May Be Higher Than Previously Reported
The new recommendations were based on a report by the U.S. Preventative Task Force (USPTF) and was the first time a major cancer organization openly admitted to the possible hazards associated with this typical conventional breast cancer screening tool. The USPTF study concluded that “changing from annual to biennial screening is likely to reduce the harms of mammography screening by nearly half.”
The “harms” that the USPTF spoke about were vague, but centered mainly around the high number of breast cancer “false positives” that are generated through initial mammogram screenings. Rightly so, “false positives” are a cause for concern.
According to a survey conducted by the Society for Women’s Health Research, a whopping 47 percent of women who received mammogram screening will get a call-back for further testing. At the same time, up to 20% of all the “tumors” doctors will detect may actually be nothing at all or cases of ductal carcinoma in situ (DCIS), which is the presence of abnormal cells inside the milk ducts of the breasts. DCIS has been classified as a “non-cancer”, and the condition is normally not a cause for further investigation or treatment.
Yet incidents of DCIS have come to represent 25% of all diagnosed Breast Cancers, since DCIS is considered by conventional standards to be “Stage 0 Breast Cancer.” According to a 2000 study conducted by the University of California, San Francisco, the risk of dying from DCIS alone within 5 years is less than 1%.
Unfortunately, all the warnings and media stories about false positives don’t appear to be curbing the number of them happening each year, nor has it cleared up the confusion around DCIS. A March 2017 Danish study found that the number of “false positives” may even be higher than earlier estimates. In their report published in the Annals of Internal Medicine, the researchers from the Nordic Cochrane Centre in Copenhagen stated that 1 in every 3 cases of invasive tumors and DCIS may represent over diagnosis. The percentage of false positives in that country may be as high as 48%.
False Positives: Just the Tip of the Iceberg
Getting a “false positive” result from a mammogram screening can lead to emotional and physical suffering caused by not only by the stress of receiving the news, but also by unnecessary biopsy, surgery, chemo and radiation. But this only scratches the surface when it comes to the possible “harms” caused by mammogram screenings.
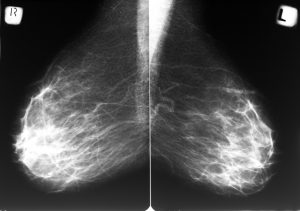
Studies point to the fact that mammograms may actually be a cause of both DCIS and breast cancer. The number of DCIS cases reported in the U.S. rose from less than 2 per 100,000 in the 1980’s to roughly 33 per 100,000 in 2004.
This correlates with the increasing emphasis on mammograms as the “breast cancer screening tool of choice” which began at the end of the 1980’s. Tissue around the breast area is sensitive and all the poking and prodding that goes along with a mammogram can easily aggravate the area.
In addition, a 2006 study published in the British Journal of Radiology discovered that the radiation used in a normal mammogram can be up to six times more damaging to the sensitive cells of the breast area than higher-level x-rays since the radiation will accumulate in the body with each yearly or biennial exam. And 2014 report published in that same journal also expressed concerns with repeated exposure to doctor-derived radiation.
According to the researchers from Columbia University Medical Center in New York:
“Concerns arise when CT examinations are used without a proven clinical rationale, when alternative modalities could be used with equal efficacy, or when CT scans are repeated unnecessarily.”
The amount of radiation a patient is exposed to in a mammogram screening is about the same as a typical CT scan.
You Have A Choice
Even though the news is finally getting out about some of the risks of mammograms, it will still take a while for the news to sink in for the general public. In the meantime, take heart! There ARE ways to be proactive with prevention and also stay safe in the process. Choosing to use the amazing technology of Thermography as well as specific and sensitive blood work are a few major ways to be proactive. In next week’s blog, we’ll explore what Thermography is and why it is so effective for early detection, as well as some other tests you can take advantage of to not only check your breast cancer risk, but the state of your overall health as well.
Dr. Veronique Desaulniers, better known as Dr. V, is the founder of The 7 Essentials System ™, a step-by-step guide that teaches you exactly how to prevent and heal Breast Cancer Naturally. To get your F.R.E.E. 7 day mini e-course, and to receive her weekly action steps and inspiring articles on the power of Natural Medicine, visit https://breastcancerconqueror.com/.

Excellent article.Thank you.
Thermograms are available widely. Check your area for a clinic at http://www.meditherm.com
Take care, ladies,
Ann
I noticed that major hospitals such as Boston Medical Center in the Boston, MA area do not offer thermography yet automatically suggest mammography (harmful radiation and potential damaging compression to ductal tissues/tumor pockets). This is rather sad, as Boston is known to be a one of the best cities to travel to when in need of medical help.
My gynecologist told me today that I should stay away from thermography. ???? I am not getting a mammogram that they want me to get. I asked for an ultrasound instead, but she basically told me I’d most likely be denied. Anyway, I found your article today and am glad! Thank you!
You are so very welcome Emily! I am glad that this article has helped you in some way! Remember, it is your health! So do your research and do what feels right to you.
I stopped having mammograms 7 years ago; I am now 73. Have had a thermogram every year instead. This year I knew something wasn’t right and showed the thermogram tech what I noticed. She noticed too and requested a quicker result. The results showed “within normal limits” (Jan’17). By June, the lump had grown and I went in for a mammogram; they immediately did an ultrasound, then a biopsy. Then I had a PEM/Pet scan and the result showed stage II, ER positive 99%, PR positive 100%, infiltrating lobular carcinoma.
So, when I talked to the thermogram people they apologized; said sometimes errors are made and obviously this was an error. So, thermograms don’t always pick up cancers.
I would advise that if you find a lump and the thermogram says its normal, then go get a second test.
Hello Helen!
Thank you so much for sharing your story. There is absolutely no screening test that is 100%. So you are right! It is very important that you get multiple opinions.